Preventing “identity theft” in prostate cancer cells re-sensitizes them to therapy
UTSW study suggests combination therapy might help prostate cancer patients overcome resistance to current treatments
DALLAS – Oct. 18, 2022 – Stopping prostate cancer cells from morphing into other cell types can overcome the resistance they develop to widely prescribed therapies, a study led by UT Southwestern scientists suggests. The findings, published in Nature Cancer, could lead to a new approach to fight this deadly disease, the second-most common cancer in American men that kills nearly 35,000 annually in the U.S.
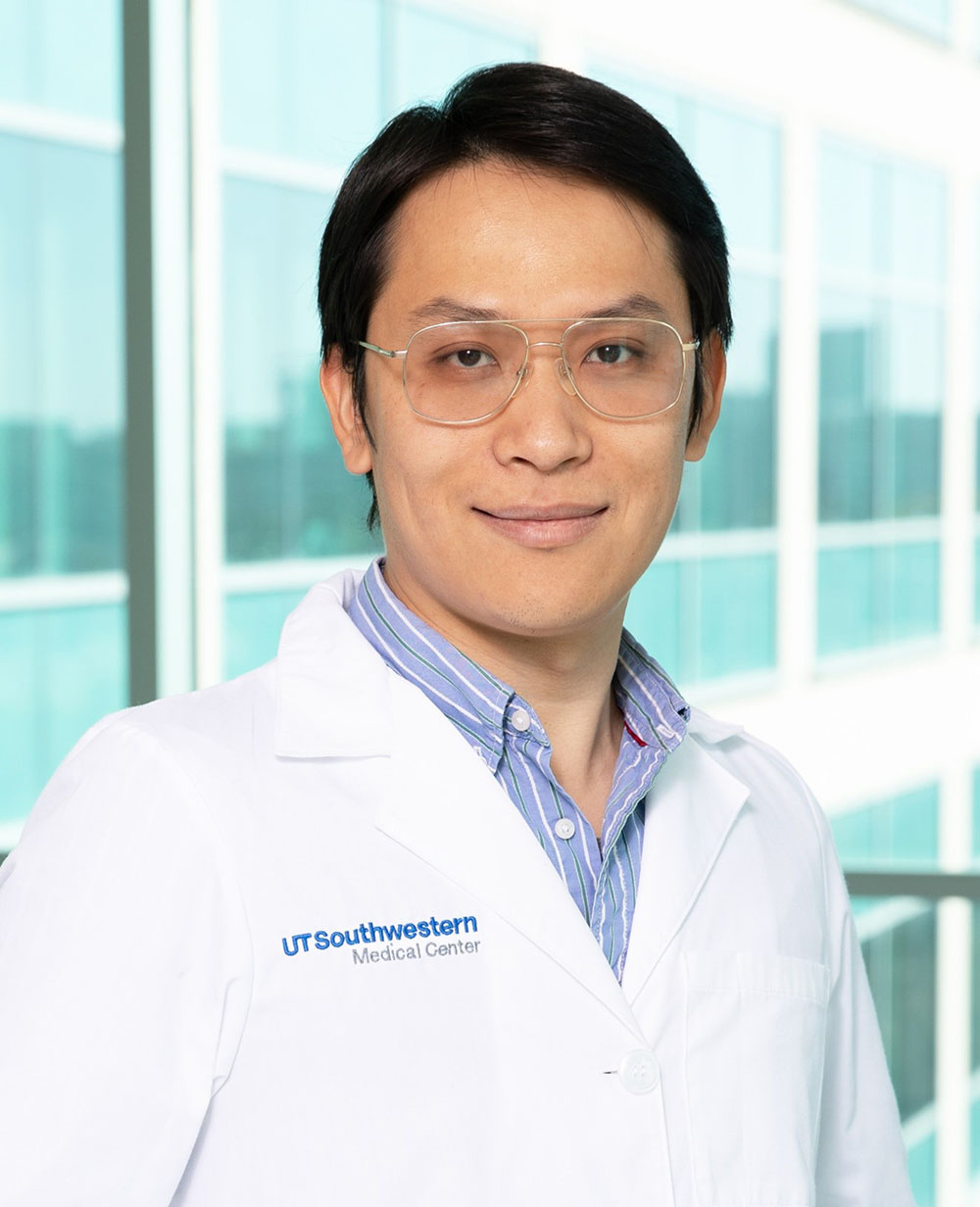
“We think this novel combination therapy could dramatically improve clinical outcomes of prostate cancer patients and hopefully save many lives,” said study leader Ping Mu, Ph.D., Assistant Professor of Molecular Biology and a member of the Harold C. Simmons Comprehensive Cancer Center.
Drugs that target the androgen receptor (AR), a key protein for prostate development and maintenance, have revolutionized prostate cancer management in recent decades, extending the lives of hundreds of thousands of patients. However, explained Dr. Mu, these therapies fail over time as prostate tumors develop resistance to them.
In the past five years, Dr. Mu and other cancer researchers discovered that one reason these tumors become resistant is through a phenomenon called lineage plasticity, in which malignant prostate cells revert to an earlier stage in development and take on a new identity, becoming a different cell type that no longer depends on the AR. Although lineage plasticity has been discovered in other cancer types, including lung cancer, breast cancer, and melanoma, the molecular mechanism behind it has remained largely unknown, stymieing efforts to develop therapies to prevent resistance from developing.
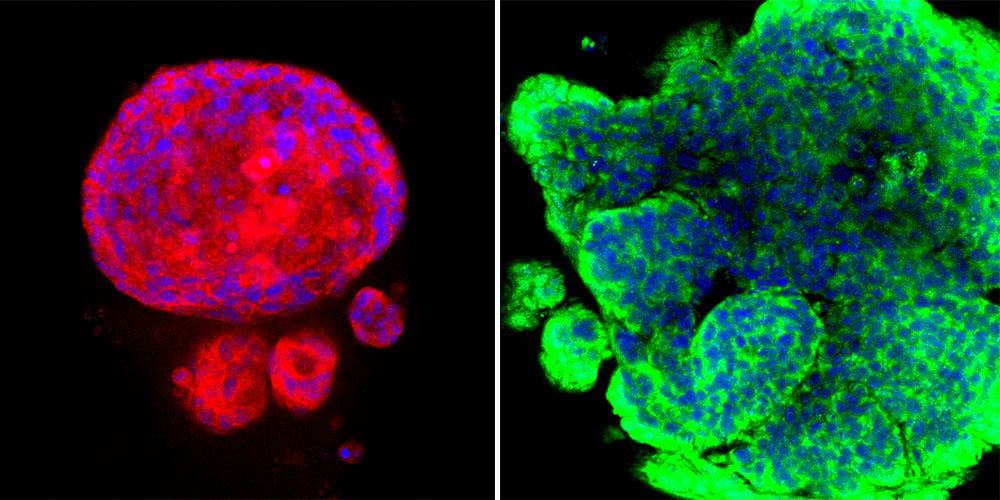
To better understand what drives lineage plasticity and resistance, Dr. Mu and his colleagues compared cells that were resistant and sensitive to AR-targeting drugs using multiple lab models: human prostate cancer cell lines growing in petri dishes, three-dimensional “organoids” made of human and mouse prostate cancer cells that mimic the structure of natural prostate cancers, and mouse models of prostate cancer. Using different analytical methods including single-cell RNA sequencing, the researchers searched for key molecular pathways that separated the resistant cells from the sensitive ones.
Their search revealed that a particular signaling pathway called Janus kinase-signal transducer and activator of transcription (JAK-STAT) appeared to drive both lineage plasticity and resistance. When the researchers used a genetic technique to separately knock out the 11 major genes that make up this pathway, they discovered that genes known as JAK1 and STAT1 played key roles in these phenomena. Eliminating these genes caused cancerous prostate cells that had shifted into new cell types to revert to their original identities and become sensitive to current therapy again.
Treating cancer cells with drugs that inhibit these genes had a similar effect, Dr. Mu explained, not only ending their lineage plasticity but also re-sensitizing them to AR-targeting therapies. When resistant prostate cancer cells were treated with both JAK1 and STAT1 inhibitors along with an AR-targeting drug, these cancer cells lost their ability to divide and survive.
Using a similar strategy could offer a new way to overcome resistance in human prostate cancer patients, Dr. Mu said, an approach he and his colleagues plan to eventually test in a clinical trial.
Other UTSW researchers who contributed to this study include Su Deng, Choushi Wang, Yunguan Wang, Yaru Xu, Xiaoling Li, Nickolas A. Johnson, Atreyi Mukherji, U-Ging Lo , Julisa Gonzalez, Lauren A. Metang, Jianfeng Ye, Carla Rodriguez Tirado, Kathia Rodarte, Zhiqun Xie, Carlos Arana, Valli Annamalai, Xihui Liu, Douglas Strand, Bo Li, Ganesh Raj, Tao Wang, and Jer-Tsong Hsieh.
Dr. Mu is a Deborah and W. A. “Tex” Moncrief, Jr. Scholar in Medical Research at UTSW.
This work was supported or partially supported by the National Cancer Institute/National Institutes of Health (5R00CA218885 and 1R37CA258730, 1P30CA142543, 1R01CA258584, 1R01CA245318, R01CA178431, and T32C124334), the Department of Defense (W81XWH-18-1-0411, W81XWH21-1-0520, W81XWH-16-1-0474, and W81XWH2110418), the Cancer Prevention and Research Institute of Texas (RR170050, RP220473, RP190208, RR170079, and RP160157), the Prostate Cancer Foundation (17YOUN12), The Welch Foundation (I-2005-20190330), the UTSW Deborah and W. A. Tex Moncrief, Jr., Scholar in Medical Research Award, the UTSW Harold C. Simmons Comprehensive Cancer Center Pilot Award, and the UTSW CCSG Data Science Shared Resource.
About UT Southwestern Medical Center
UT Southwestern, one of the nation’s premier academic medical centers, integrates pioneering biomedical research with exceptional clinical care and education. The institution’s faculty has received six Nobel Prizes, and includes 24 members of the National Academy of Sciences, 18 members of the National Academy of Medicine, and 14 Howard Hughes Medical Institute Investigators. The full-time faculty of more than 2,900 is responsible for groundbreaking medical advances and is committed to translating science-driven research quickly to new clinical treatments. UT Southwestern physicians provide care in more than 80 specialties to more than 100,000 hospitalized patients, more than 360,000 emergency room cases, and oversee nearly 4 million outpatient visits a year.
