Study suggests key to antipsychotic drug-induced obesity
UT Southwestern-led team finds possible mechanism behind weight gain, other metabolic disorders along with potential to neutralize their effects
DALLAS – Jan. 08, 2024 – An increased concentration of the hormone leptin in fat cells is believed to be responsible for weight gain associated with antipsychotic drugs, according to research led by UT Southwestern Medical Center. The study, published in Science Translational Medicine, used a mouse model to uncover the underlying mechanisms of unwanted metabolic side effects and to test an antibody that might reduce them.
Despite the effectiveness of antipsychotic drugs in managing psychiatric conditions, prescriptions such as olanzapine and risperidone can cause patients to add significant weight and in some cases result in diabetes and liver disease.
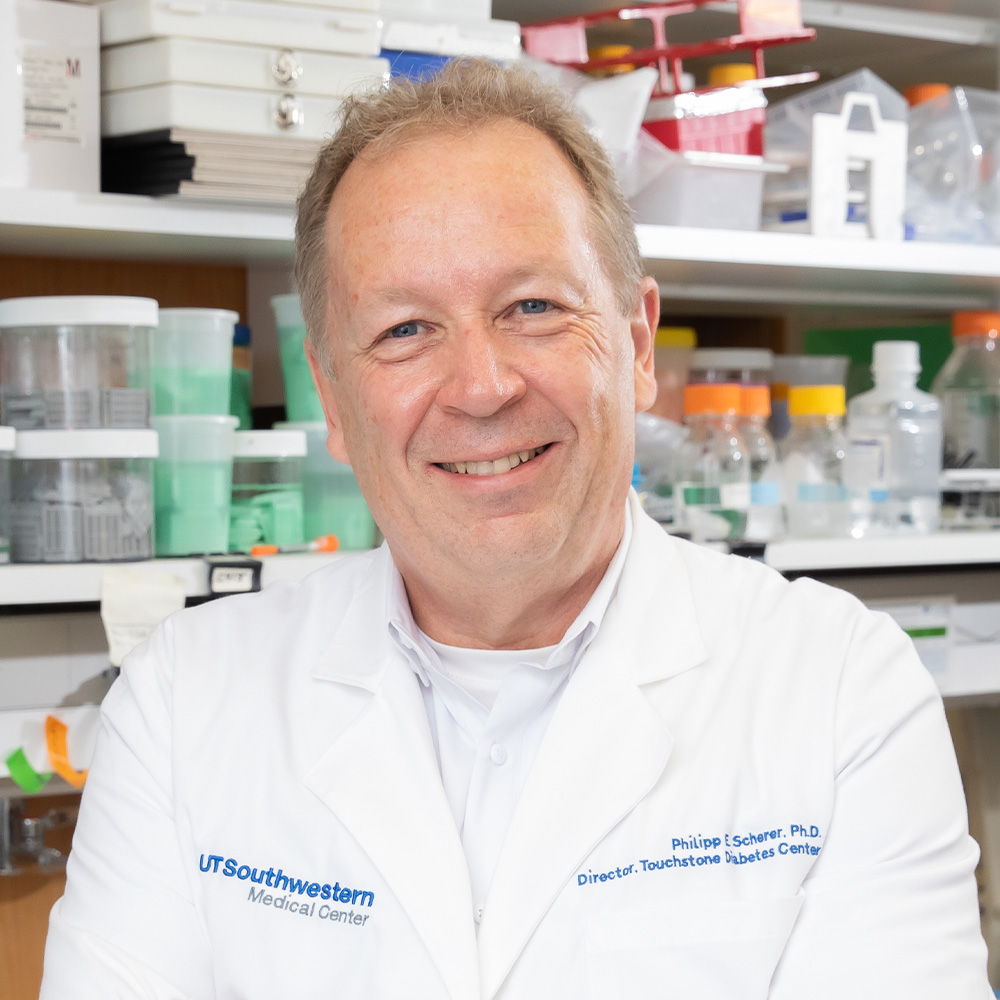
“Weight gain affects most patients who start taking these antipsychotic drugs and is a well-established side effect of these interventions. As a result, many individuals become insulin resistant and diabetic. The study implicates leptin as a key driver of these negative metabolic consequences,” said Philipp Scherer, Ph.D., Professor of Internal Medicine and Director of the Touchstone Center for Diabetes Research at UT Southwestern.
Patients using antipsychotic drugs experience increased concentrations of circulating leptin released from fat cells before they begin to gain weight. Prior to this study, however, it was not well understood how increased leptin, or hyperleptinemia, was connected to this drug-induced weight gain.
“While it was historically viewed as a ‘passenger’ to obesity – meaning levels go up as we gain weight – our data strongly suggest that it is a ‘driver’ for drug-induced obesity,” Dr. Scherer explained.
Using a previously tested mouse model, researchers obtained evidence that hyperleptinemia was directly contributing to obesity and issues such as liver fibrosis, insulin resistance, and untimely mammary duct development. Moreover, researchers found that hyperleptinemia increased inflammation, which is considered a main contributor in the development of antipsychotic drug-induced metabolic disorders.
Results also indicated that treating mice with a leptin-neutralizing antibody greatly reduced the side effects. Treatment with the antibody led to reduced weight gain, inflammation, and mammary gland development as well as improved glucose tolerance in mice with drug-induced side effects. These key findings provide a path toward improving outcomes for patients in the future.
“We are working hard to take the leptin-neutralizing antibodies that we have used here into a clinical setting to find out whether the mechanisms defined in rodents also apply to individuals who embark on an antipsychotic treatment regimen,” Dr. Scherer noted.
Other UTSW researchers who contributed to this study include co-first authors Shangang Zhao, Ph.D., former postdoctoral researcher, and Qian Lin, Ph.D., postdoctoral fellow, both in the Touchstone Center; Joel K. Elmquist, D.V.M., Ph.D., Professor of Internal Medicine, Pharmacology, and Psychiatry, Director of the Center for Hypothalamic Research, and Vice Chair of Research for Internal Medicine; Associate Professor Chen Liu, Ph.D., Assistant Professors May-Yun Wang, Ph.D., and Christine M. Kusminski, Ph.D., Instructors Qingzhang Zhu, Ph.D., and Chao Li, Ph.D., and Assistant Instructor Steven C. Wyler, Ph.D., all of Internal Medicine; Li Li, Ph.D., postdoctoral research fellow at the Center for Hypothalamic Research; Leon Straub, Ph.D., and Jan-Bernd Funcke, Ph.D., both postdoctoral fellows in the Touchstone Center; Xue-Nan Sun, Ph.D., postdoctoral fellow in the Oh Lab; and Shiuhwei Chen, M.S., Senior Research Associate at the Touchstone Center.
Drs. Elmquist and Liu are Investigators with the Peter O’Donnell Jr. Brain Institute.
Dr. Scherer holds the Gifford O. Touchstone, Jr. and Randolph G. Touchstone Distinguished Chair in Diabetes Research and the Touchstone/West Distinguished Chair in Diabetes Research. Dr. Elmquist holds the Carl H. Westcott Distinguished Chair in Medical Research and the Maclin Family Distinguished Professorship in Medical Science, in Honor of Dr. Roy A. Brinkley. Dr. Zhao holds a Voelcker Fund Young Investigator Pilot Award from the Max and Minnie Tomerlin Voelcker Fund.
This study was funded by grants from the National Institutes of Health (R01-DK55758, R01-DK099110, RC2-DK118620, R01-DK127274, R01-DK131537, P01-AG051459, R01-DK118725, R01-DK088423, R01 DK114036, DK130892, and R00-AG068239), Cancer Prevention and Research Institute of Texas (RP190561), American Heart Association (23POST1019715 and 855170), and funding from the UT Southwestern Nutrition Obesity Research Center under the National Institute of Diabetes and Digestive and Kidney Diseases and the National Institutes of Health (P30-DK127984).
About UT Southwestern Medical Center
UT Southwestern, one of the nation’s premier academic medical centers, integrates pioneering biomedical research with exceptional clinical care and education. The institution’s faculty members have received six Nobel Prizes and include 26 members of the National Academy of Sciences, 21 members of the National Academy of Medicine, and 13 Howard Hughes Medical Institute Investigators. The full-time faculty of more than 3,100 is responsible for groundbreaking medical advances and is committed to translating science-driven research quickly to new clinical treatments. UT Southwestern physicians provide care in more than 80 specialties to more than 120,000 hospitalized patients, more than 360,000 emergency room cases, and oversee nearly 5 million outpatient visits a year.
