UTSW scientists eliminate key Alzheimer’s feature in animal model
Study suggests possible way to prevent memory-robbing disease
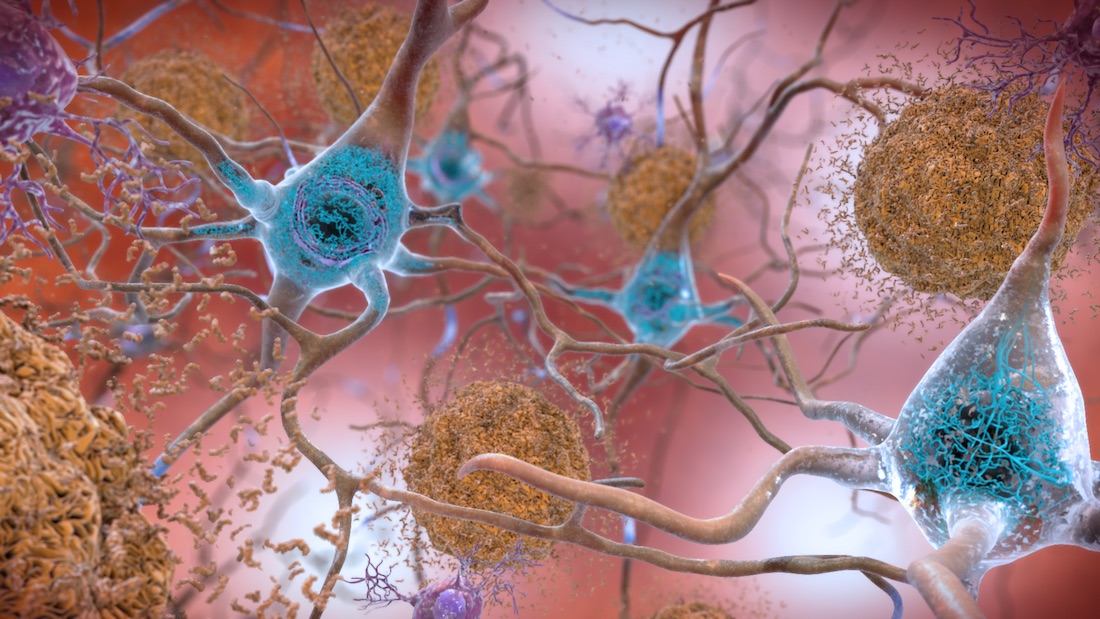
Credit: National Institute on Aging, National Institutes of Health
DALLAS – Oct. 28, 2021 – A study by UT Southwestern researchers finds that changing the biochemistry of parts of brain cells abolished the formation of amyloid beta plaques in a mouse model of Alzheimer’s disease. The finding, published in eLife, might eventually lead to treatments that prevent the memory-robbing condition in humans.

“We envision that drugs that act on the same protein we inhibited in these mice could someday play a similar role in Alzheimer’s disease as statins do in heart disease, helping to prevent the condition from ever developing,” said Joachim Herz, M.D., Professor of Molecular Genetics, Neurology, and Neuroscience at UTSW. Dr. Herz led the study, and graduate student Connie Wong was a co-lead author.
Nearly 6 million Americans have Alzheimer’s disease, with the vast majority developing a late-onset form that arises after age 65. Alzheimer’s disease is characterized by brain cells plagued by extracellular plaques made of a protein called amyloid beta and intracellular tangles made of an abnormal form of a protein called tau. Although the causes of the disease are not well defined, scientists have long known that the most significant genetic risk factor for late-onset Alzheimer’s is apolipoprotein E4 (ApoE4), one of three variants of a protein involved in fat metabolism in mammals. In humans, having the ApoE4 variant reduces the average age of Alzheimer’s onset by several years compared with having the most common variant, ApoE3, while rarer ApoE2 appears to have a protective effect against this disease.

The three versions of ApoE are very similar structurally, Ms. Wong explained: Compared with ApoE2, ApoE3 contains one amino acid substitution, resulting in that protein having a more positive charge. The ApoE4 variant contains two amino acid substitutions, resulting in the highest positive charge of the three forms of ApoE protein. The mechanism by which these differences affect late-onset Alzheimer’s risk has been unknown.
In their new study, Dr. Herz, Ms. Wong, and their colleagues homed in on early endosomes, organelles responsible for sorting proteins, recycling them for reuse, or transporting them through the cell interior to cellular garbage dumps called lysosomes. Previous research had shown that early endosomes are enlarged in people and animals with ApoE4, compared with those who carried the other two ApoE variants.
Using genetically modified mice that model Alzheimer’s disease and produce the human forms of ApoE4 and amyloid beta, the researchers showed that the positive charges on ApoE4 caused this protein to clump inside early endosomes because the charge of ApoE4 matches that of the environment inside endosomes. This clumping prevents these organelles from continuing their journey through the cell to transport, recycle, or help dispose of other proteins, including amyloid beta.
However, when the researchers used a genetic technique to turn off a gene called NHE6 in brain cells, they found that the negative effects of ApoE4 were eliminated, and the protein was transported through the cell without impediment. NHE6 produces a protein that acts as a pH regulator for endosomes, exchanging acidic protons for sodium ions. When the researchers shut off the NHE6 gene, removing its protein from the cell, the early endosomes quickly became more acidic and that biochemical change seemed to prevent amyloid beta aggregation.
“Inhibiting NHE6 produced the same protective effect as having ApoE2, an effect we hope can eventually be replicated using pharmaceuticals,” Ms. Wong said.
The team plans to continue to study this mechanism and how to inhibit NHE6 in future studies.
Current and former UTSW researchers who contributed to this study include co-lead authors Theresa Pohlkamp, now at Regeneron Pharmaceuticals, and Xunde Xian, now at Peking University, as well as Murat S. Durakoglugil, Gordon Chandler Werthmann, Bret M. Evers, Charles L. White III, Jade Connor, and Robert E. Hammer. Takaomi C. Saido of the Riken Center for Brain Science also contributed.
This work was supported by the National Institutes of Health (grants R37 HL063762, R01 NS093382, R01 NS108115, and RF1 AG053391, as well as 1F31 AG067708-01 from the National Institute on Aging), the Darrell K Royal Research Fund, the BrightFocus Foundation (A20135245, A2016396S); the Harrington Discovery Institute; a Circle of Friends Pilot Synergy Grant; and the Bluefield Project to Cure FTD.
Dr. Herz holds the Presbyterian Village North Foundation Distinguished Chair in Alzheimer’s Disease Therapeutic Research and the Thomas O. and Cinda Hicks Family Distinguished Chair in Alzheimer’s Disease Research.
About UT Southwestern Medical Center
UT Southwestern, one of the nation’s premier academic medical centers, integrates pioneering biomedical research with exceptional clinical care and education. The institution’s faculty has received six Nobel Prizes and includes 25 members of the National Academy of Sciences, 16 members of the National Academy of Medicine, and 14 Howard Hughes Medical Institute Investigators. The full-time faculty of more than 2,800 is responsible for groundbreaking medical advances and is committed to translating science-driven research quickly to new clinical treatments. UT Southwestern physicians provide care in about 80 specialties to more than 117,000 hospitalized patients, more than 360,000 emergency room cases, and oversee nearly 3 million outpatient visits a year.
