Scan for arterial plaque is better at predicting heart attack than stroke
Study examined predictive value of coronary calcium scores for heart attack and stroke in men and women and among different races
DALLAS – Aug. 18, 2020 – The amount of calcified plaque in the heart’s arteries is a better predictor of future heart attacks than of strokes, with similar findings across sex and racial groups, according to new research from UT Southwestern.
The study, published today in Circulation: Cardiovascular Imaging, is the first to examine the predictive value of recently recommended coronary artery calcium (CAC) score categories for heart attacks and strokes. Using two population-based, multiethnic cohorts, the researchers evaluated how well the amount of calcium detected by a CT scan of the heart predicted whether white, Black, and Hispanic men and women would have a stroke or a heart attack in the next 10 years.

Calcium is part of the fatty plaque that builds up in arteries supplying blood to the heart and brain and can lead to blockages, causing heart attacks or strokes. As plaque becomes more calcified and hardens, it becomes more visible on a heart CT scan.
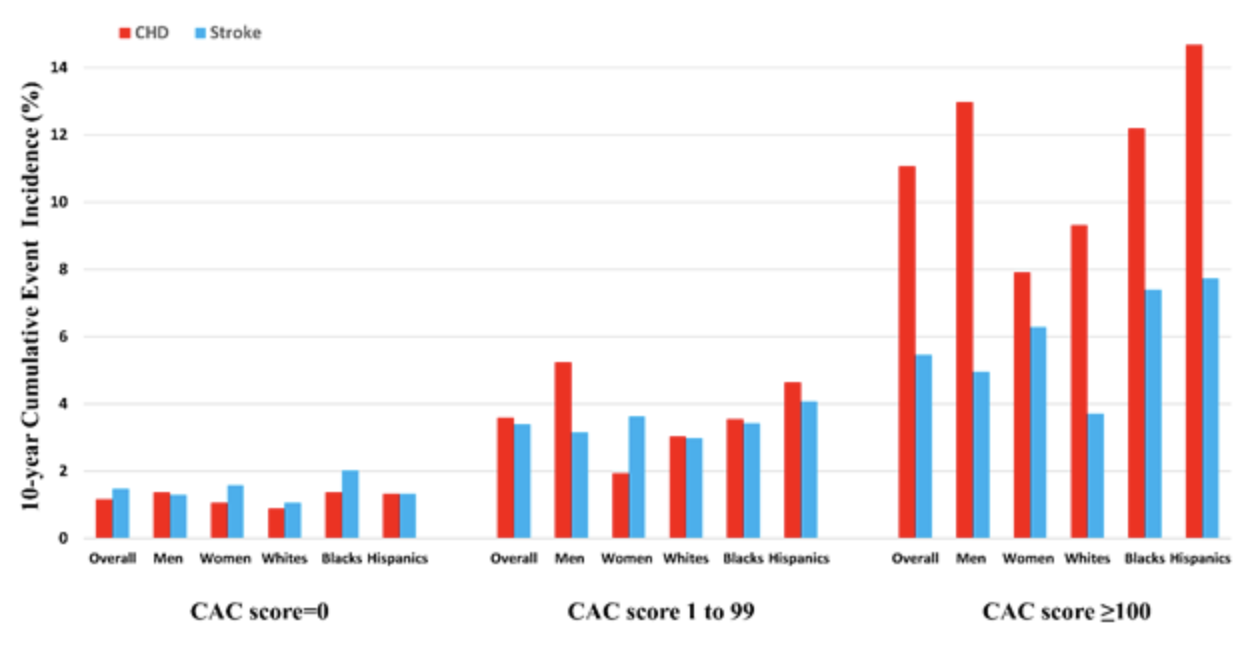
“In our study, there was a twofold greater risk of heart attack than stroke at CAC levels at or above 100,” a score indicating moderate to high levels of calcified plaque, says Parag Joshi, M.D., a cardiologist and assistant professor of internal medicine at UT Southwestern and senior author of the study. “That held true for Black, white, and Hispanic men and women.”
Women and Black individuals generally have higher stroke risk, Joshi says.
“In fact, while the calcium score may not be a strong predictor of stroke risk for most, for some reason it did well in predicting strokes in Black participants,” says Anurag Mehta, M.D., the first author of the study, formerly at UT Southwestern and now at Emory University School of Medicine.
The findings could help guide health care providers as they decide how aggressively to treat patients with risk factors such as high cholesterol and blood pressure but who have never had a major cardiovascular event.
In 2018, the American Heart Association and the American College of Cardiology issued joint cholesterol management guidelines that recommend using the CAC score as an aid when deciding whether to prescribe a cholesterol lowering statin drug in situations where the decision – based on the routine risk assessment using systolic blood pressure, cholesterol level, etc. – is uncertain.
Joshi’s study evaluated data from more than 7,000 participants in two large studies – the Multi-Ethnic Study of Atherosclerosis (MESA) funded by the National Institutes of Health, and the Dallas Heart Study at UT Southwestern.
The authors divided study participants by the AHA/ACC calcium risk categories – 0, 1-99, and 100 or above – to evaluate how useful the calcium scores would have been in predicting heart attacks and strokes. It also subdivided the participants by sex and race (Black, white, and Hispanic) to calculate the risk levels for the different groups.
For participants with a calcium score of zero, there was a similarly low risk of either a stroke or a heart attack in the coming 10 years – less than 2 percent for either event among all study participant categories, according to the study.
The risk level for both heart attacks and strokes rose a bit for those with scores of 1-99, yet still remained below 6 percent – increasing about equally for both and across most demographic groups. At this level, women did have a greater increase in the risk for stroke than for heart attack, whereas men had higher heart attack risk than stroke.
Greater differences were found when the CAC scores rose to 100 or above, with heart attack risk twice as high as stroke risk for the entire study population. While 10-year heart attack risk jumped above 12 percent for men and over 14 percent for Hispanic individuals, heart attack risk for women was approximately 8 percent, according to the study.
Meanwhile, stroke risk remained below 8 percent across all groups, although women, Black, and Hispanic people had higher risk than men and white participants.
For doctors and patients, the findings could help tilt the scales either toward or away from using statin drugs to lower cholesterol in cases where the decision is not clear-cut from factors such as age, sex, cholesterol, systolic blood pressure, and smoking history.
Patients are sometimes reluctant to begin what is likely to become a lifelong drug therapy, Joshi says. “If you think your patient should be on a statin and your patient doesn’t want to take it, this can be a good arbitrator of that,” he says. “Our findings also highlight some of the nuance between heart attack risk and stroke risk and how our patients might consider those two risks in their decision-making.”
Researchers at Emory University School of Medicine, Johns Hopkins Bloomberg School of Public Health, Johns Hopkins School of Medicine, Johns Hopkins Ciccarone Center for the Prevention of Cardiovascular Disease, the University of California Los Angeles Medical Center, and Houston Methodist Hospital participated in the study.
Funding was provided by the National Heart, Lung, and Blood Institute; the National Center for Advancing Translational Sciences; and the Donald W. Reynolds Foundation. Some researchers received awards, grants, or fees from the American Heart Association, the Abraham J. & Phyllis Katz Foundation, Novo Nordisk, Sanofi/Regeneron, GlaxoSmithKline, AstraZeneca, Pfizer, Bayer, or Regeneron. Joshi holds equity interest in Global Genomics Group.
About UT Southwestern Medical Center
UT Southwestern, one of the premier academic medical centers in the nation, integrates pioneering biomedical research with exceptional clinical care and education. The institution’s faculty has received six Nobel Prizes, and includes 24 members of the National Academy of Sciences, 16 members of the National Academy of Medicine, and 13 Howard Hughes Medical Institute Investigators. The full-time faculty of more than 2,500 is responsible for groundbreaking medical advances and is committed to translating science-driven research quickly to new clinical treatments. UT Southwestern physicians provide care in about 80 specialties to more than 105,000 hospitalized patients, nearly 370,000 emergency room cases, and oversee approximately 3 million outpatient visits a year.
