The cutting edge
Scientists on cusp of solving genetic diseases by snipping defective DNA
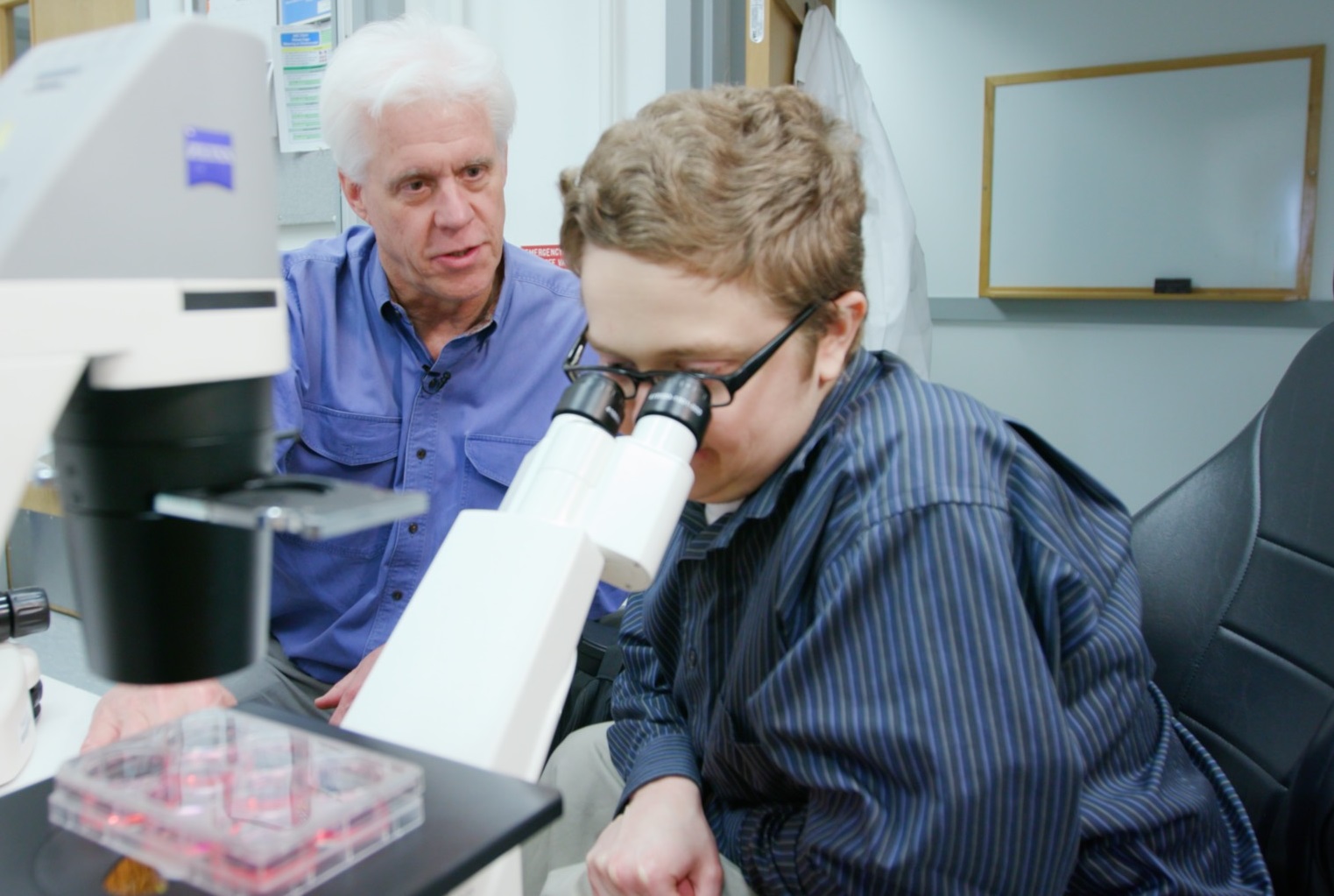
DALLAS – April 25, 2019 – Ben Dupree peered through the microscope at the beating heart cells, awestruck by the implications.
These were his cells, edited in the lab to correct a genetic flaw that had caused his muscles to deteriorate since childhood, forced him into a wheelchair, and perpetuated the prospects of an early death from Duchenne muscular dystrophy (DMD).
Yet, here he witnessed a breakthrough that changed the narrative, a realization that after years of despair and depression, a lifesaving treatment for his condition was no longer a far-fetched dream.
“It’s unbelievable,” Mr. Dupree, 26, said as he looked at his cells during a recent visit to a UT Southwestern gene-editing lab. “This could save so many lives one day.”
Advancements in gene editing, buoyed by the discovery of CRISPR technology that enables precise editing of the human genome, have put scientists on the cusp of solving some of mankind’s most devastating and baffling disorders. Among them is DMD, a muscle-withering disease that UT Southwestern geneticists have halted in animals and human cells through a single-cut gene-editing technique.
The next major step: a clinical trial that could change the prognosis for the most common fatal genetic disease in children and perhaps set the stage to treat other deadly diseases.
“Duchenne muscular dystrophy is a holy grail of genetic diseases, and we’re so close now to helping people like Ben,” said Dr. Eric Olson, an expert in genetic engineering at UT Southwestern. “Once we make headway with this condition, CRISPR in principle could be used for almost any disease in which we know the error in the DNA.”
A rare mutation
Diagnosed at age 9, Mr. Dupree has spent most of his life dealing with the demoralizing effects of DMD. He recalls, even before diagnosis, the daunting task of keeping up with other children during soccer games or school exercise.
“Other kids would be running around, and I would be sitting with my hands on my knees trying to catch my breath,” he said. “It was hard to go through that.”
His family later learned this was far more serious than a lack of athleticism. Soon he was struggling to get up the stairs. Standing became a strenuous effort.
At the urging of an occupational therapist, Mr. Dupree’s mother sought neuromuscular testing and a biopsy that returned disturbing results: He had a rare genetic mutation that prevents his body from producing dystrophin, a protein that acts like a shock absorber for heart and muscle fibers when they expand and contract. Without dystrophin, the boy’s muscle fibers were falling apart – a condition that leads to muscle and heart failure and death by the early 30s, often much earlier.
Debbie Dupree did her best to hide the prognosis from her son as she began researching what could be done. She read about the latest findings on DMD, traveled to conferences, and met with doctors and other families dealing with the disease. Meanwhile, the boy’s muscles continued to deteriorate, and by middle school he was using a wheelchair full time.
“When a doctor tells you your child will most likely be gone within a decade because there is no treatment, you go into shock,” Mrs. Dupree said. “But I needed to educate myself. … Watching him struggle and continue to weaken is heartbreaking.”
‘Patient Zero’
Mrs. Dupree, who had not heard of Duchenne before her son showed signs of the disease, was dismayed to learn of the lack of immediate options for DMD patients. Yet hope remained. Scientists had known for decades that DMD is caused by a defect in any of the 79 exons that comprise the dystrophin gene, and medical technology had recently reached a point that these defects could potentially be corrected through gene editing.

Coincidentally, one of the world’s leading experts on muscle disease who lived in Mr. Dupree’s neighborhood was researching this very strategy. Dr. Olson invited Mr. Dupree to UT Southwestern in 2015 to give a blood sample to test whether a new CRISPR method his lab developed could work on human cells.
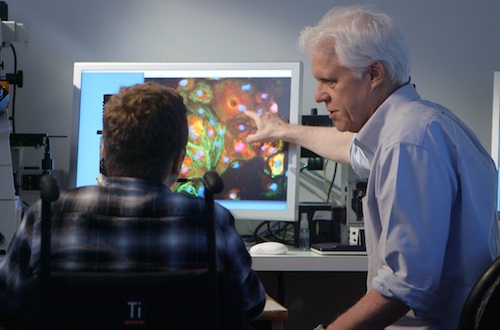
Dr. Olson’s team followed a series of biochemical steps to convert the sample into heart cells and used CRISPR to correct the exon defect and restore dystrophin. The team then invited Mr. Dupree to see the results through the microscope.
“That was one of the most inspiring moments of the work, to see Ben’s face when he saw his cells beating in a dish, producing the dystrophin that his body cannot make,” Dr. Olson said. “He was our Patient Zero. Now the challenge is to adapt the technique to safely deliver the gene-editing components into the human body.”
A different approach
Dr. Olson’s work is a notable part of a series of programs at UT Southwestern aimed at developing genetic treatments for muscle diseases and a number of ultra-rare neurological conditions largely overlooked by the medical field.
UT Southwestern is trailblazing a series of clinical trials for the latter in which a single healthy gene missing from the patient’s DNA can be packaged into a harmless virus and delivered into cells. But scientists had to devise a different approach for DMD because the dystrophin gene – one of the largest in the human body – cannot fit inside the virus.
Dr. Olson’s team developed a CRISPR-Cas9 technique to fix the gene instead of adding a healthy copy into the cells. The technique requires two components: an enzyme called Cas9 that cuts DNA and a guide RNA that functions like a molecular GPS device to direct Cas9 to the specific exon to be edited.
Cas9 and the RNA are each loaded into an adeno-associated virus (AAV), with the RNA directing the Cas-9 to the mutated exon where it snips the DNA. The editing process bypasses the mutation and enables muscle fibers to produce dystrophin, with positive results documented in studies by Dr. Olson in dogs, mice, and human cells.
Success with these treatments could lay the foundation for the more intricate gene therapies of common conditions – from epilepsy to autism – involving multiple genes that are either mutated or missing. But for now Dr. Olson’s team is focused on saving patients like Mr. Dupree, one of about 300,000 children in the world with DMD.
“We’ve come a long way,” said Dr. Olson, whose lab has since edited cells taken from other patients with different exon mutations. “If someone had told me four years ago we’d be able to halt the progression of muscular dystrophy in a dog with a single injection of a virus with CRISPR, I would not even have understood what they were saying.”
Mental strife
Mr. Dupree has come a long way as well. He overcame early mental strife to become a vocal advocate for DMD research and takes pride in helping younger patients deal with the complexities that lie ahead.
But he acknowledges scars from the anguish he felt growing up with a terminal disease – the difficulties of watching his body weaken throughout his childhood, seeing the same horrifying effects in other DMD patients who have since passed away.
His teenage years in particular – a time of growing independence for most youths – was a period of increasing frustration as the disease complicated many facets of his life. While playing in the high school band, for instance, he often had to sit away from the group because parts of the stadium weren’t wheelchair accessible. He soon gave it up, as he did many other activities that reminded him of his physical demise.
“I was very depressed,” Mr. Dupree said. “I think that at age 15, 16, kids want to try to be independent. They really struggle with the idea of relying on other people. I had to come to terms with that.”
A new purpose
Mr. Dupree’s disposition began to change in college, after accepting his mother’s invitation to join her on trips to speak with other families across the country dealing with DMD. He soon met with youngsters with the same issues he had experienced the last several years.
Here he found a purpose beyond lamenting his own situation. He became a comforting source of perspective and encouragement for parents and children wondering how to cope with the disease and what steps they could take to further efforts to develop a cure.
“I was able to come out of that dark place through the community of support,” Mr. Dupree said. “The people I came to know fostered a feeling that we’re all in this together and that brought me back to where I am today.”
Setting an example
Mr. Dupree exudes a genuine love of life’s simple joys: He smiles as he talks of traveling the country and of other hobbies such as cooking and astronomy. He laughs heartily as he watches home videos with his mother, reminiscing about a family vacation when he played a game of chase with his younger sister.


He still keeps in touch with Dr. Olson, discussing the latest in science and sharing personal stories as well. It’s a relationship built on mutual respect and admiration, two people who are overcoming challenges to reach their ultimate goals.
“From the first time I met Ben, I felt we had a real connection,” Dr. Olson said. “It is probably surprising to people who realize many scientists will work their entire lives on a disease and not know someone personally who has that disease.”
Mr. Dupree continues to devote much of his time to helping others. He earned a bachelor’s degree in biochemistry – with the initial aim of researching DMD – and is now seeking a master’s in social work to counsel those with disabilities.
“I struggled a lot with accepting my diagnosis,” he said. “I’m hoping to use social work training to more directly help people get through what I’ve gone through.”
Mr. Dupree is an example to DMD patients. He has found ways to live as independently as possible. He has learned to drive and cook, and when he needs to, he’ll ask for help.
Regarding the prospects of overcoming DMD, Mr. Dupree takes nothing for granted.
“I’m not necessarily hoping for a cure but for anything that could slow the progression of the disease,” he said. “Even if I’m not here to see the lifesaving treatment, my hope is that people being born now with the disease can still benefit.”
About Dr. Olson
Dr. Olson is Director of UT Southwestern’s Hamon Center for Regenerative Science and Medicine, and Professor and Chair of Molecular Biology. He holds the Pogue Distinguished Chair in Research on Cardiac Birth Defects, the Robert A. Welch Distinguished Chair in Science, and the Annie and Willie Nelson Professorship in Stem Cell Research. He is also the founder of Exonics Therapeutics Inc., launched in February 2017 to advance and commercialize his research.
His studies are supported, in part, by Exonics Therapeutics Inc. and grants from the National Institutes of Health, the Sen. Paul D. Wellstone Muscular Dystrophy Cooperative Research Center, The Robert A. Welch Foundation, Parent Project Muscular Dystrophy, and CureDuchenne.
Disclosure statements: Dr. Eric Olson is a scientific co-founder of, and consultant for, Exonics Therapeutics and has license and investment interests with the company.
About UT Southwestern Medical Center
UT Southwestern, one of the premier academic medical centers in the nation, integrates pioneering biomedical research with exceptional clinical care and education. The institution’s faculty has received six Nobel Prizes, and includes 22 members of the National Academy of Sciences, 17 members of the National Academy of Medicine, and 15 Howard Hughes Medical Institute Investigators. The full-time faculty of more than 2,500 is responsible for groundbreaking medical advances and is committed to translating science-driven research quickly to new clinical treatments. UT Southwestern physicians provide care in about 80 specialties to more than 105,000 hospitalized patients, nearly 370,000 emergency room cases, and oversee approximately 3 million outpatient visits a year.






